4. Longevity and a new fitting model
4.1 Introduction
An attempt is made to develop a fitting model based on an acceptable partial use of the dynamic range of hearing. Audibility of normal conversational speech, with its 30 dB wide speech range, is an important factor in that model.
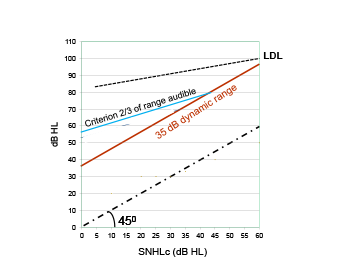
A new goal has been formulated: at least 35 dB of the dynamic range of hearing should be accessible with a device; that means that with proper amplification conversational speech is audible (Zwartenkot et al., 2014 and Rheinfeldt et al., 2015). This criterion is indicated in Figure 4.1. The idea is that 35 dB HL is enough to hear conversational speech adequately while the amplifying hearing device makes use of wide-dynamic range compression with slow release times, thus is working as an automatic volume control. This criterion is referred to as the ‘DR>35 dB rule’. A second criterion is now introduced, namely at least 2/3 of the dynamic range of hearing should be audible with a minimum of 35 dB (referred to as the ‘DR 2/3 rule’). This criterion is based on the data of Figure 3.2. Baha patients in that study were fitted with different types of linear devices with volume wheel. Typically, their aided dynamic range of hearing equals about 2/3 of the unaided range, at least up to 30 dB HL. This new criterion is illustrated by the blue line in Figure 4.1.
Table 4.1 presents the MPO data from Table 2.1. The third and fourth columns of this table indicate up to what mean SNHLc value the different devices fulfill the ‘DR>35 dB rule” or ‘the DR 2/3”. These values deviate from those advocated by most manufacturers.
Figure 4.1. The minimal desired mean MPO versus mean SNHLc. Red line presents the minimal desired MPO if the aided dynamic range of hearing has to be 35 dB at least (DR>35 dB rule). The blue line gives such target values if at least 2/3 of the dynamic range should be audible with a minimum of 35 dB (DR 2/3 rule).
Amongst others, Table 4.1 suggests that the Sophono Alpha 1 device can be used in conductive hearing loss: indeed Sylvester et al. (2013) came to a similar conclusion, using sound field measurements and speech tests. The Table further suggests that the percutaneous BCDs (with their most powerful processors) and the VSB device have approximately the same capacity. Previously, Bosman et al. (2006) advocated 65 dB HL as the upper limit for the Baha Cordelle. They used a different criterion, namely, speech perception should be 50% or better and they showed that, on the average, the criterion was fulfilled by patients with a SNHLc of up to 50 dB HL. They further argued that as there was no alternative (but CI), the Baha Cordelle device could be used with some benefit in patients with SNHLc of up to 60-65 dB HL.
Table 4.1
| Device | MeasuredMPO* | Max SNHLc if the ‘DR 2/3 rule’ is used | Max SNHLc if the “DR>35 dB rule” is used |
| Sophono Alpha 1 | 53 dB HL | 5 dB HL | 20 dB HL |
| Bonebridge | 63 dB HL | 20 dB HL | 30 dB HL |
| Standard Baha Divino/BP100 | 67 dB HL | 25 dB HL | 30 dB HL |
| Standard Ponto | Idem | 25 dB HL | 30 dB HL |
| Baha 5SP | 85 dB HL | 50 dB HL | 50 dB HL |
| Vibrant Soundbridge | 85 dB HL | 50 dB HL | 50 dB HL |
| Codacs ** | 100 dB HL | >65 dB HL | >65 dB HL |
| Baha Attract/BP110 | 64 dB HL | 20 dB HL | 30 dB HL |
* taken from Table 2.1
** no longer available
When using the milder criterion (DR>35 dB rule), the application ranges are broader, see fourth column. As was argued, a working range of 30 or 35 dB might be just enough in combination with wide-dynamic range compression device (Rheinfeldt et al., 2015). Wide dynamic range compression is the standard choice for patients with pure sensorineural hearing loss using BTEs who have an obvious limited dynamic range of hearing because of physiological conditions. Indeed, using wide dynamic range compression is an option here; however, the better option is to choose a device with a higher MPO. Especially in children, powerful devices should be used, see Chapter 5.
The ‘DR 2/3 rule’ is based on the choices made by a group of Baha users; therefore better defined than the ‘DR>35 dB rule’. However, there is room for further refinements.
It should be noted that the Max SNHLc values per device type, as presented in the table, are in agreement with maximum SNHLc values as obtained from clinical studies, as presented in Figure 3.3.c. Using the trend-curves indicated in that figure, the maximum SNHLc per device type could be defined as well (viz. 45 dB HL for VSB and 15-20 dB HL for the transcutaneous BCDs). Importantly, the resemblance between these values and those presented in the Table 4.1 validates the MPO based Max SNHLc values as presented in the table.
Concerning the use of hearing devices for conductive and mixed hearing loss, the limited MPO has to be taken into account. Patients compensate for a low MPO by lowering the gain of the device, leading to an unintended decrease in perception of speech. In short, today’s passive transcutaneous BCDs can be used in patients with normal cochlear function or with a limited SNHLc, the active Bonebridge device in patients with SNHLc below 25 dB HL, percutaneous BCDs and VSB in patients with SNHLc up to 50 dB HL. These values are more conservative than those claimed by the manufacturers and might change when more powerful processors are released.
4.2. Longevity
What about longevity? Owing to aging or a progressive cochlear disease, the SNHLc will deteriorate over time. Using data on age-related hearing deterioration enables the estimation of ‘years of effective use’ of a particular device. As an example, Figure 4.2 shows data of patients with otosclerosis (type OTSC7). Iliadou et al. (2006) studied the mean hearing loss deterioration (air- and bone-conduction thresholds) as a function of age for such patients. The first line of the figure shows the age and the second line the mean SNHLc (0.5, 1, 2 and 4 kHz averaged) as published by Iliadou et al. Iliadou et al. presented data up to age 60; the data at 70 and 80 years are extrapolated as indicated by the i after the SNHLc value. The thick red lines indicate whether or not a certain device can (still) be used according to ‘DR 2/3 rule’. E.g. when using the Baha data from Table 4.1 (Baha usable up to SNHLc of 45 dB HL), it can be seen that this device can be used up to approx. age 75 years. The Ponto device with its most powerful processor can also be used lifelong. As well as the VSB.
Probably, the mildest scenario is that of some patient with a stable conductive hearing loss component and additionally presbycusis. Using the median age-related hearing deterioration for men, taken from ISO 7029, figure 4.3 is obtained.
Figure 4.2. Effective device use for a patient with progressive hearing loss owing to otosclerosis (OTSC7), based on the ‘DR 2/3 rule’. SNHLc stands for the cochlear hearing loss of patients
Figure 4.3. Effective device use for a patient with stable conductive hearing loss component and a sensorineural component that deteriorates over time owing to presbycusis. The ‘DR 2/3 rule’ was applied
Again, the percutaneous BCD device and the VSB device seem to be the better choice.
When choosing for a particular treatment, longevity is one of the factors that should be considered. The expected degree of hearing deterioration over time should be assessed from the patient’s history.
It should be noted that the conclusion drawn from Table 4.1 and Figures 4.2 and 4.3 are valid for the specified device types. If more powerful audioprocessor are released, conclusions will change.
Longevity is an often ignored but important factor when counseling treatment options, especially when surgery (implantation) is involved.
4.3 Attempt to formulate a prescription procedure
So far, the evaluation of the capacity of various amplification options concerned the MPO as a low MPO restricts the aided dynamic range of hearing of the patient. To deal with that limitation, compression is often used. It should be noted that compression affects the aided thresholds positively, overestimating the gain provided by the device. A second limiting factor might be audible microphone noise; patients with predominant conductive hearing loss might hear device noise, owing to their (sub) normal cochleae. Then expansion can be used to make the noise inaudible (Dillon, 2012), however, expansion affects the aided thresholds negatively, under-estimating the gain provided by the device. The noise level of a device should be clearly indicated on datasheets, which is only the case for percutaneous BCDs. A documented measuring procedure is available. Although problems with the noise floor have been reported with the VSB processors (e.g. Linder et al., 2009), according to the manufacturer, problems with the Amade soundprocessor are minor and expansion is not used. For the Cochlear Codacs device, the noise floor is approximately 40 dB HL standard (Cochlear’s data sheets), which can be lowered to 25 dB HL and should be explicitly taken into account when considering this device for a patient.
To choose the best device for a given patient is important. Note that when considering the application of a middle ear implant, well-masked bone-conduction thresholds are essential to ensure that the cochlea of the to-be-implanted ear is sensitive enough for successful application of the implant. On the other hand, for the application of BCDs, unmasked bone-conduction thresholds of the to-be-treated ear should be considered. Owing to the limited transcranial attenuation of bone vibrations, the BCD will stimulate the cochlea with the best sensitivity, which might be either the ipsilateral or contralateral cochlea (Stenfelt, 2012). Consequently, the fitting should be based on the unmasked bone-conduction thresholds.
Regarding device fitting, it should be realized that either an implantable BCD or a middle-ear implant with its actuator coupled to one of the cochlear windows, directly stimulate the cochlea, bypassing the impaired middle ear. Therefore, the efficacy of the sound processor fitting depends directly on how well the cochlear loss (or SNHLc), as expressed by the bone-conduction thresholds, is compensated. This simply implies that we can build on our knowledge of fitting conventional hearing devices (e.g. BTEs) in pure sensorineural hearing loss. Desired gain and desired output values can be determined by using validated prescription rules developed for sensorineural hearing loss, like the classical half-gain rule (HGR; often used as a rule of thumb) or the more sophisticated NAL and DSL rules (Dillon, 2012).
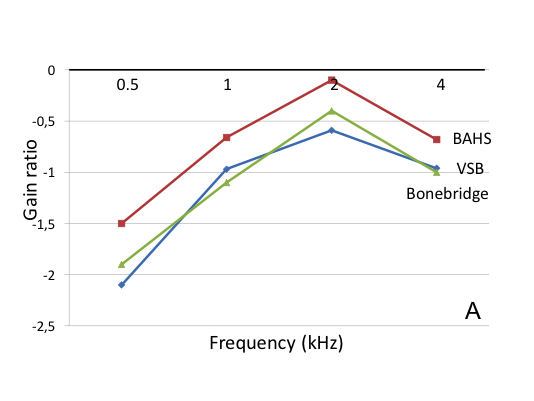
To develop a practice-based prescription procedure, we studied published data. The 24 selected studies, introduced in Chapter 3, were used once more. For each of these studies, the gain at cochlear level was calculated as a function of frequency. That gain, referred to as ‘effective gain’, is by definition the frequency specific bone-conduction threshold (cochlear threshold) minus the aided threshold (for more information, see Appendix 2.3). To obtain a relative gain value, corrected for the degree of hearing loss, the ‘effective gain’ was divided by the bone-conduction threshold, referred to as the gain ratio. According to the above-mentioned rule of thumb (half-gain-rule), that ratio should be 0.5 (with some minor corrections; Dillon, 2012).
Twenty of the 24 papers provided all the data needed for such calculations and were included. Figure 4.4 presents the gain ratios, presented per device type and the degree of cochlear loss (SHNLc). To deal with the discontinuities seen in Figures 3.2, 3.3 and 3.3.c, the 20 studies were divided into 3 subgroups, according to the mean SNHLc of the participants. Group 1 comprised the studies in patients with a mean SNHLc below 25 dB HL, group 2 those with SNHLc between 25 and 40 dB HL and group 3 those with a SNHLc exceeding 40 dB HL; see Table 4.2. Using Table 4.1 and noise level data, for each subgroup, the amplification options are added, third row.
Table 4.2. Subgroups to deal with the discontinuities observed in Figure 3.2
| Group 1 | Group 2 | Group 3 | |
| Mean SNHLc | < 25 dB HL | 25 to 40 dB HL | > 40 dB HL |
| Figure 3.2 shows: | Negative gain | Intermediate | Positive gain |
| Amplification options based on Table 4.1 and noise floor data | Percutaneous BCD/VSB/Bonebridge | Percutaneous BCD/VSB | Percutaneous BCD/VSB/Cochlear MET? |
| Hypothetical target for gain | Predominant conduc-tive loss: compensate the air-bone gap! | Intermediate | ‘Compensate’ the SNHLc as if it was a pure sensorineural loss |
Furthermore, using Table 4.1 and noise level data, for each subgroup, the amplification options are listed.
Lines in Figure 4.4 are labeled according to device type.
Figure 4.4. The gain ratio (gain divided by threshold) as a function of frequency. Figure 4.4A presents the data of group 1 (BAHS stands for Baha and Ponto together: 1 study, n=20; VSB: 3 studies, n=34 and Bonebridge: 1 study, n=12), Figure 4.4B for group 2 (BAHS: 6 studies, n=113; VSB: 7 studies, n=97) and Figure 4.4C for group 3 (BAHS: 1 study, n=12; VSB: 3 studies, n=47).
Obviously, Figure 4.4 shows that all the gain ratios are below 0.5, the prescribed value according to the half gain rule. That rule is more or less outdated. More dedicated rules have been developed, like the NAL rule (Dillon, 2012). Typically, the gain ratio using that rule is lower than 0.5.
The figure also shows that the gain ratio is the highest at 2 kHz, irrespective of device type and subgroup. Furthermore, it is evident that inter-group differences are large (compare subfigures A, B and C). Differences between devices within groups are less outspoken.
These data have been used to develop the practice-based prescription procedure: for mixed hearing loss, it is assumed that the cochlear loss should be ’compensated’ as in sensorineural hearing loss. For predominant conductive hearing loss, the air-bone gap should be compensated; thus the gain (and thus the gain ratio) should be (close to) 0. However, negative gain ratios are seen (Figure 4.4.A). As suggested by Dillon (2012) and discussed in Chapter 1, maybe not the whole air-bone gap has to be compensated but only partially. It is suggested, based on our data, that the aided thresholds should be better than 25 dB HL for those patients with (sub) normal cochlear function. More details are found in Snik et al., 2019.
Table 4.3 presents the target aided thresholds and target effective gain, following the principles of the NAL prescription rule and the data presented in Figure 4.4. A margin of 5 dB has been taken into account.
Table 4.3. Target values as a function of SNHLc for 1, 2 and 4 kHz
|
SNHLc (dB HL) |
0 |
10 |
20 |
30 |
40 |
50 |
60 |
|
Target aided threshold (dB HL) |
<25 |
<25 |
<25 |
<25 |
<25 |
<27 |
<33 |
|
Effective gain (aided minus cochlear thresholds dB) |
-25 |
-15 |
-5 |
5 |
15 |
23 |
27 |
Following the NAL rule, gain at 0.5 kHz might be set 10 dB lower than that at the higher frequencies as indicated in the table, resulting in target aided thresholds that are 10 dB higher than those listed in the table (Snik, et al, 2019).
What are the limitations of this proposed procedure? It should be noted that this evaluation is based on today’s hearing implants. Furthermore, the procedure has not (yet) been validated. However, the gain ratios for Codacs device, a very powerful device (3 studies, 43 participants, see paragraph 5.3.2, mean SNHLc = 55 dB HL) were: 0.35, 0.40 and 0.22 for the frequencies 1 to 4 kHz, which exceed the values for the other devices (Figure 4.4), approaching but still below the proposed target values for 1 and 2 kHz.
This practice-based prescription procedure can be used irrespective of the type of device used. Prerequisite is that a device is chosen with sufficiently high MPO, according to Table 4.1, preferably following the ‘DR 2/3 rule’.
Importantly, note that for percutaneous BCDs, Hodgetts and Scollie (2017) developed a dedicated prescription rule, based on the DSL fitting rule. That procedure is the preferred option, taking, amongst others, the limited MPO of these BCDs into account.